Cornea Treatment
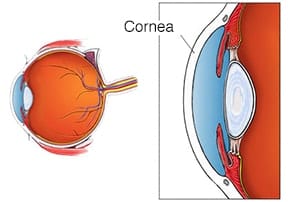
The cornea is the clear covering on the front of the eye which bends, or refracts, light rays and focus them on the retina in the back of the eye. When a cornea is damaged or diseased, its ability to correctly focus these rays can be compromised.
Sometimes, the curvature of the corneal is too severe for correction through glasses or contact lenses. A thorough eye exam is needed to diagnose these disorders. Our corneal specialists will work with you to find the best solution to treat these disorders and to help preserve your vision.
Corneal Transplant
Corneal transplantation (keratoplasty) is recommended when curvature is too severe to be treated with other methods, or when extensive damage has occurred due to disease, infection or injury. Some of the more common problems that may require transplantation are:
- Fuch’s Corneal Dystrophy
- Bullous Keratopathy
- Keratoconus
- Corneal Ulceration
- Herpes Simplex Keratopathy
- Central Corneal Scar
- Corneal Dystrophies such as Lattice, Granular or Macular Dystrophy
- Traumatic injury
- Chemical Burn
Transplantation involves replacing the damaged cornea with a healthy one from a donor (usually through an eye bank). There are two types of Corneal Transplants: Full thickness corneal transplant or Penetrating Keratoplasty (PKP) and Lamellar Keratoplasty. Keratoplasty is a low-risk procedure – it is the most common type of transplant surgery and has the highest success rate.
Keratoconus / Corneal Cross-Linking
Keratoconus, often referred to as ‘KC’, is a non-inflammatory eye condition in which the typically round dome-shaped cornea progressively thins and weakens, causing the development of a cone-like bulge and optical irregularity of the cornea. This causes ‘static’ in your vision and can result in significant visual impairment.
Keratoconus typically first appears in individuals who are in their late teens or early twenties, and may progress for 10-20 years, and then slow or stabilize. Each eye may be affected differently. In the early stages of keratoconus, people might experience:
- Slight blurring of vision
- Distortion of vision
- Increased sensitivity to light
The cornea is responsible for focusing most of the light that comes into the eye. Therefore, abnormalities of the cornea, such as keratoconus, can have a major impact on how an individual sees the world, making simple tasks such as driving a car or reading a book very difficult.
Cross-linking is a minimally invasive outpatient procedure that combines the use of UVA light and riboflavin eye drops to add stiffness to corneas which have been weakened by disease or refractive surgery. Cross-linking, which has been performed in Europe since 2003, is considered the standard of care around the world for keratoconus and corneal ectasia following refractive surgery.
- Creates new corneal collagen cross-links
- Results in a shortening and thickening of the collagen fibrils
- Leads to the stiffening of the cornea
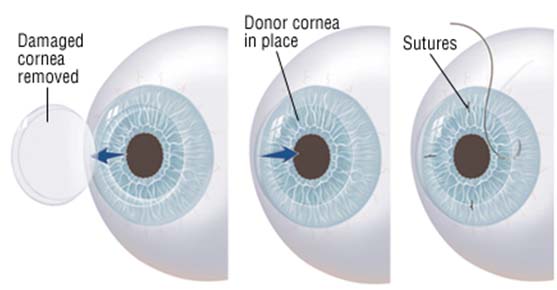
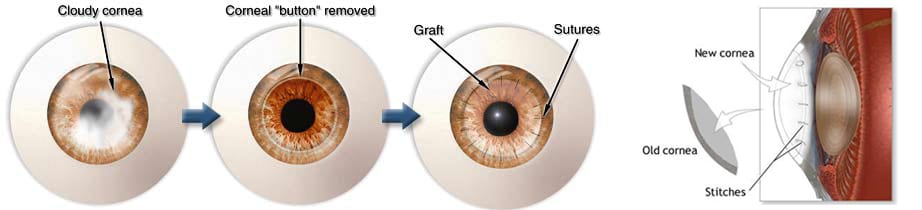
PKP
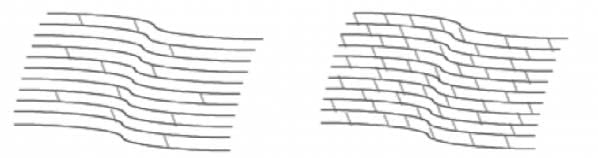
Full thickness corneal transplants, also known as penetrating keratoplasty (PKP), are used for corneas with disease extending through all layers of the cornea. During the procedure a circular incision is made in the cornea. A disc of tissue is removed and replaced with a similar sized disc of donor tissue. Sutures are used to secure the donor tissue in place. Local or general anesthesia may be used. The procedure lasts 60-90 minutes. Careful follow-up is necessary post-operatively to ensure good healing and to prevent corneal transplant rejection.
Lamellar Keratoplasty
The second type of corneal transplant is a Lamellar Keratoplasty in which only the diseased portion of the cornea is removed and replaced with donor tissue. DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty) is an example of this and is the most common lamellar procedure performed. Because DSAEK replaces only the diseased posterior section of the patient’s cornea, the procedure requires minimal suturing and provides patients with more rapid visual restoration, less discomfort and a reduced risk of sight-threatening complications. This procedure generally takes 45 minutes, is performed under local anesthesia and requires careful follow-up care to ensure good healing and to prevent the rejection of the transplanted tissue.