Retina
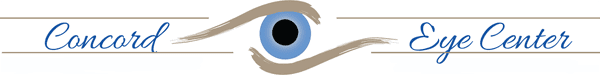
The retina is a thin sheet of nerve tissue in the back of the eye, where light rays are focused and images are transmitted to the brain. The center of the retina is called the macula. The vitreous is a gel-like substance that fills the eye and is attached to the retina in several areas including the macula and the optic nerve.
Problems with the retina can take different forms and treatments also vary. The vitreous can separate from the retina. This is called a posterior vitreous detachment (PVD). The majority of PVD’s have an uncomplicated course.
However, in a small percentage of patients, problems with the retina may develop after a PVD, such as a retinal tear, retinal detachment, epiretinal membrane, or a macula hole. These issues generally need treatment fairly quickly to avoid vision loss.
Diabetes creates conditions that can also negatively impact one’s vision and diabetics should be particularly vigilant about having regular eye exams with a board-certified retinal specialist like the ones at Concord Eye Center.
Posterior Vitreous Detachment
A Posterior Vitreous Detachment (PVD) is a condition of the eye in which the vitreous membrane separates from the retina. There are some conditions that can increase your likelihood of having a retinal detachment. They include:
- Nearsightedness
- Prior cataract surgery
- Glaucoma
- Severe injury or trauma to the eye
- A prior retinal detachment in the other eye
- A family history of retinal detachment
Some symptoms include:
- New floater or floaters in the field of vision
- Flashing or flickering lights in the field of vision
- A shadow in the periphery of your field of vision
- Blurred vision or a cloud moving across your field of vision
Retinal tears or detachments are generally treated with either lasers or surgery. These procedures can correct problems before vision is lost or prevent further deterioration from occurring.
If you experience any of the above symptoms, call us for an appointment.
Diabetic Retinopathy
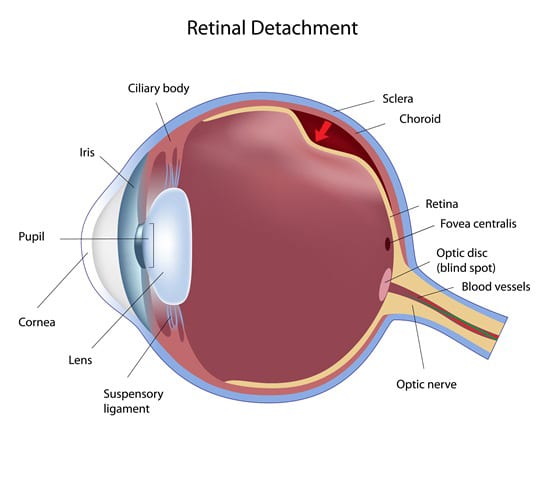
Diabetes creates conditions that can seriously affect the eyes and it is extremely important that anyone with diabetes has regular eye exams. Early detection and treatment offers the best chance of preserving vision in people with diabetic retinopathy and other eye diseases.
detection and treatment offers the best chance of preserving vision in people with diabetic retinopathy and other eye diseases.
In the United States, Diabetic retinopathy is the number one cause of blindness among people between the ages of 20 and 65. It is a serious eye condition that can develop in diabetics – it occurs when blood vessels within the eye begin to leak. The fluid leaking into the eye causes the macula (part of the retina) to swell, obscuring close vision and fine details. This first phase of diabetic retinopathy is called the nonproliferative stage.
In the proliferative stage, new blood vessels begin to form on the retina. These vessels are defective and continue to rupture and leak fluid into the eye. This can eventually lead to retinal detachment, which can cause blindness.
Aside from controlling blood sugar levels, there are several treatments available for diabetic retinopathy, including laser photocoagulation and other laser and conventional surgical procedures.
Macular Degeneration
The macula is the central area of the thin nerve layer in the back of the eye called the retina. The fovea is located in the center of the macula. This area is responsible for our sharp central vision and for vivid color vision. Macular degeneration is a serious eye disease that can lead to vision loss.
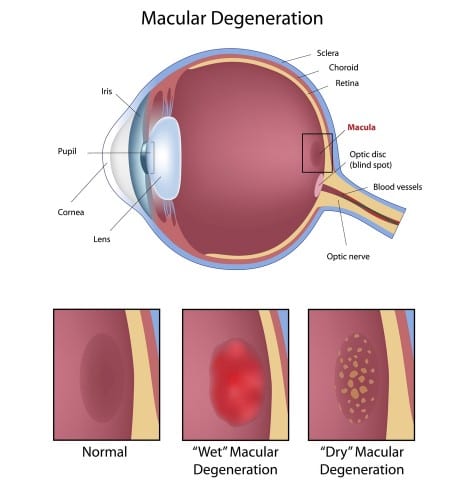
There are two forms of age-related macular degeneration (AMD). Wet AMD is more serious but also more treatable and far less common. Dry AMD is more widespread and more difficult to treat. Still, in either case, early detection is absolutely vital to preserving vision.
Causes & Symptoms
Most cases of macular degeneration are age-related. After the age of 50, there is an increased risk of developing macular degeneration during each additional decade of life. It is more common in Caucasians with fair skin and lightly colored eyes. Additional risk factors for macular degeneration include smoking, family history of AMD, high blood pressure and high cholesterol.
Wet age-related macular degeneration involves leakage and bleeding in the macula which then can cause contraction and scarring of the macula. Blood vessels break through a layer called Bruch’s membrane and then can leak or bleed. This is termed a choroidal neovascular membrane (CNVM). Wet AMD can cause a relatively sudden and significant loss or distortion of central vision.
Dry age-related macular degeneration is the most common type and represents about 90% of all cases of macular degeneration. Dry AMD involves atrophy and pigmentary changes in the macula. Often drusen or yellow-white spots are present and located beneath the retina. Mild cases may be asymptomatic, but if the atrophy affects the fovea it may cause blurred central vision and central blind spots.
Treatment
No matter which form of macular degeneration you have, it is important to be seen by a doctor as soon as possible.
Wet AMD
Wet AMD can be managed with medication, laser, or a combination of both modalities.
Our knowledgeable and experienced retinal specialists provide the latest treatment modalities for Wet AMD including laser therapy and intravitreal injections of Anti-VEGF agents, such as Lucentis, Avastin, and Eyelea.
Dry AMD
There is no cure or treatment for Dry AMD, although vitamins, antioxidants and zinc may be beneficial in slowing the progression of the disease. Over time, it is possible for the dry form to change to the wet form of the disease. This usually involves a sudden change in vision or central distortion, and should be evaluated as soon as possible.